What May Cause Achilles Tendinitis ?
Overview
 The Achilles tendon camera.gif connects the calf muscle to the heel bone. It lets you rise up on your toes and push off when you walk or run. The two main problems are, Achilles tendinopathy. This includes one of two conditions, Tendinitis. This actually means "inflammation of the tendon." But inflammation is rarely the cause of tendon pain. Tendinosis. This refers to tiny tears (microtears) in the tissue in and around the tendon. These tears are caused by overuse. In most cases, Achilles tendon pain is the result of tendinosis, not tendinitis. Some experts now use the term tendinopathy to include both inflammation and microtears. But many doctors may still use the term tendinitis to describe a tendon injury. Problems with the Achilles tendon may seem to happen suddenly. But usually they are the result of many tiny tears in the tendon that have happened over time. Achilles tendinopathy is likely to occur in men older than 30. Most Achilles tendon ruptures occur in people 30 to 50 years old who are recreational athletes ("weekend warriors"). Ruptures can also happen in older adults.
The Achilles tendon camera.gif connects the calf muscle to the heel bone. It lets you rise up on your toes and push off when you walk or run. The two main problems are, Achilles tendinopathy. This includes one of two conditions, Tendinitis. This actually means "inflammation of the tendon." But inflammation is rarely the cause of tendon pain. Tendinosis. This refers to tiny tears (microtears) in the tissue in and around the tendon. These tears are caused by overuse. In most cases, Achilles tendon pain is the result of tendinosis, not tendinitis. Some experts now use the term tendinopathy to include both inflammation and microtears. But many doctors may still use the term tendinitis to describe a tendon injury. Problems with the Achilles tendon may seem to happen suddenly. But usually they are the result of many tiny tears in the tendon that have happened over time. Achilles tendinopathy is likely to occur in men older than 30. Most Achilles tendon ruptures occur in people 30 to 50 years old who are recreational athletes ("weekend warriors"). Ruptures can also happen in older adults.
Causes
Tight or tired calf muscles, which transfer too much of the force associated with running onto the Achilles tendon. Not stretching the calves properly or a rapid increase in intensity and frequency of sport training can make calf muscles fatigued. Activities which place a lot of stress on the achilles tendon, such as hill running and sprint training, can also cause Achilles Tendinitis. Runners who overpronate (roll too far inward on their feet during impact) are most susceptible to Achilles Tendinitis. Runners with flat feet are susceptible to Achilles Tendinitis because flat feet cause a 'wringing out' effect on the achilles tendon during running. High arched feet usually absorb less shock from the impact of running so that shock is transferred to the Achilles tendon. Use of inappropriate footwear when playing sport or running e.g., sandals, can also put an extra load on the Achilles tendon. Shoes are now available that have been designed for individual sports and provide cushioning to absorb the shock of impact and support for the foot during forceful movements. Training on hard surfaces e.g., concrete, also increases the risk of Achilles Tendinitis. Landing heavily or continuously on a hard surface can send a shock through the body which is partly absorbed by the Achilles tendon. A soft surface like grass turf helps to lessen the shock of the impact by absorbing some of the force of the feet landing heavily on the ground after a jump or during a running motion.
Symptoms
Symptoms of Achilles tendinitis and tendinosis include recurring localized heel pain, sometimes severe, along the achilles tendon during or after exercise. Pain often begins after exercise and gradually worsens. Morning tenderness or stiffness about an inch and a half above the point where the Achilles tendon is attached to the heel bone. Sluggishness in your leg. Mild to severe swelling. Stiffness that generally diminishes as the tendon warms up with use.
Diagnosis
On examination, an inflamed or partially torn Achilles tendon is tender when squeezed between the fingers. Complete tears are differentiated by sudden, severe pain and inability to walk on the extremity. A palpable defect along the course of the tendon. A positive Thompson test (while the patient lies prone on the examination table, the examiner squeezes the calf muscle; this maneuver by the examiner does not cause the normally expected plantar flexion of the foot).
Nonsurgical Treatment
Make sure that the tendon is not torn through and through. If it is severed, you must see a doctor immediately so that the tendon can be repaired. Severe injuries can sever a tendon, without a skin laceration being present. Testing involves moving the toes and foot to see if the tendon moves. If the tendon does not appear to move, it may be severed (comparing the injured tendon and its movement to the same tendon on the uninjured foot may help). Very sharp pain, a sudden pop, or an obvious gap in the structure of the tendon are all signs of a rupture, and should be seen by a doctor as soon as possible. If there is extreme swelling of the leg, and pain (out of proportion to the amount of trauma received), you may have sustained a vascular injury. A doctor must see this type of injury immediately. If you are not sure, see a doctor. If you have multiple injured areas see a doctor immediately, in order to prevent excessive swelling and pain. If the above exam is negative, then you may proceed with self-treatment. (However, if you are not sure of the extent of your injury, you should consult your doctor immediately). The sooner you begin to treat your injury by following "R.I.C.E.", the better you will feel. Rest is very important. Take off your shoe, get off your feet, and relax. Ice should be applied as soon as possible. Never apply ice directly on the injured area, as the cold may make the pain worse. Ice should be applied close to the injured site, between the heart and the injury, so that as the blood flows under the ice, it will be cooled. This cool blood flowing into the injured area will help to reduce the swelling and pain. Apply the ice, wrapped in a cloth or over an elastic bandage, to the foot for 15 minutes, every 1-2 hours, for up to 3 days after an injury. If the ice is uncomfortable, or causes increased pain, do not continue to use it, and see a doctor. If you have poor circulation do not use ice, as this may cause a serious problem. c. Compression is used to limit swelling, and to give support to the injured area. Compression should be applied to the entire foot, starting first at the toes and working back to the ankle. If it is applied just to the injured area, increased swelling will occur in front and behind the wrapping. Compression should be applied with a 3-inch elastic bandage, beginning around the base of all the toes, and then going around the foot and ankle. Continue over the calf muscle when possible. Compression reduces motion in the injured area and foot, and this decreases the pain, and allows for quicker healing. The bandage should not be so tight that it causes increased pain or throbbing in the toes or foot. It should be comfortable! Do not remove the elastic bandage for the first 12 hours, unless it becomes too tight, or the pain increases, or the toes become pale, blue, or cool. If any of these things happen, immediately remove all bandages, and leave them off for several hours. The normal color and temperature of the toes should return immediately. If not, see a doctor immediately! Continue until the swelling and pain subsides; it could take from several days to several weeks. d. Elevation of the leg will aid in reducing swelling and pain. Blood rushes to an injured area to bring increased blood cells, that aid in healing. Gravity will also force blood to the injured area. Too many cells and too much fluid will apply pressure to the injured nerves and tissues, and cause increased pain and delayed healing. Keep your foot elevated so that it is at least parallel to the ground, or higher if it is comfortable. Do this for at least 48 hours, or until the throbbing subsides, when you lower the leg.

Surgical Treatment
Mini-Open Achilles Tendon Repair. During a mini-open Achilles tendon repair surgery, 2 to 8 small stab incisions are made to pull the edges of the tendon tear together and suture the torn edges to repair the damage. During this procedure the surgeon will make one 3 to 4 cm long incision on the back of your ankle and 2 to 4 smaller vertical incisions around the long incision. These smaller veritical incisions are made with a pair of surgical scissors and are commonly referred to as "stab incisions". Once the incisions are opened up, the surgeon will place precise sutures with non-absorbable stitches to strengthen the damaged Achilles tendon tissue. This suturing technique reduces the amount of scar tissue on the tendon after surgery and provides better surface healing of the skin. Unlike the traditional method of an open surgery, this procedure has less risks and complications involved. To learn about all risks you may face be sure to speak to your doctor.
Prevention
Regardless of whether the Achilles injury is insertional or non-insertional, a great method for lessening stress on the Achilles tendon is flexor digitorum longus exercises. This muscle, which originates along the back of the leg and attaches to the tips of the toes, lies deep to the Achilles. It works synergistically with the soleus muscle to decelerate the forward motion of the leg before the heel leaves the ground during propulsion. This significantly lessens strain on the Achilles tendon as it decelerates elongation of the tendon. Many foot surgeons are aware of the connection between flexor digitorum longus and the Achilles tendon-surgical lengthening of the Achilles (which is done to treat certain congenital problems) almost always results in developing hammer toes as flexor digitorum longus attempts to do the job of the recently lengthened tendon. Finally, avoid having cortisone injected into either the bursa or tendon-doing so weakens the tendon as it shifts production of collagen from type one to type three. In a recent study published in the Journal of Bone Joint Surgery(9), cortisone was shown to lower the stress necessary to rupture the Achilles tendon, and was particularly dangerous when done on both sides, as it produced a systemic effect that further weakened the tendon.
 The Achilles tendon camera.gif connects the calf muscle to the heel bone. It lets you rise up on your toes and push off when you walk or run. The two main problems are, Achilles tendinopathy. This includes one of two conditions, Tendinitis. This actually means "inflammation of the tendon." But inflammation is rarely the cause of tendon pain. Tendinosis. This refers to tiny tears (microtears) in the tissue in and around the tendon. These tears are caused by overuse. In most cases, Achilles tendon pain is the result of tendinosis, not tendinitis. Some experts now use the term tendinopathy to include both inflammation and microtears. But many doctors may still use the term tendinitis to describe a tendon injury. Problems with the Achilles tendon may seem to happen suddenly. But usually they are the result of many tiny tears in the tendon that have happened over time. Achilles tendinopathy is likely to occur in men older than 30. Most Achilles tendon ruptures occur in people 30 to 50 years old who are recreational athletes ("weekend warriors"). Ruptures can also happen in older adults.
The Achilles tendon camera.gif connects the calf muscle to the heel bone. It lets you rise up on your toes and push off when you walk or run. The two main problems are, Achilles tendinopathy. This includes one of two conditions, Tendinitis. This actually means "inflammation of the tendon." But inflammation is rarely the cause of tendon pain. Tendinosis. This refers to tiny tears (microtears) in the tissue in and around the tendon. These tears are caused by overuse. In most cases, Achilles tendon pain is the result of tendinosis, not tendinitis. Some experts now use the term tendinopathy to include both inflammation and microtears. But many doctors may still use the term tendinitis to describe a tendon injury. Problems with the Achilles tendon may seem to happen suddenly. But usually they are the result of many tiny tears in the tendon that have happened over time. Achilles tendinopathy is likely to occur in men older than 30. Most Achilles tendon ruptures occur in people 30 to 50 years old who are recreational athletes ("weekend warriors"). Ruptures can also happen in older adults.
Causes
Tight or tired calf muscles, which transfer too much of the force associated with running onto the Achilles tendon. Not stretching the calves properly or a rapid increase in intensity and frequency of sport training can make calf muscles fatigued. Activities which place a lot of stress on the achilles tendon, such as hill running and sprint training, can also cause Achilles Tendinitis. Runners who overpronate (roll too far inward on their feet during impact) are most susceptible to Achilles Tendinitis. Runners with flat feet are susceptible to Achilles Tendinitis because flat feet cause a 'wringing out' effect on the achilles tendon during running. High arched feet usually absorb less shock from the impact of running so that shock is transferred to the Achilles tendon. Use of inappropriate footwear when playing sport or running e.g., sandals, can also put an extra load on the Achilles tendon. Shoes are now available that have been designed for individual sports and provide cushioning to absorb the shock of impact and support for the foot during forceful movements. Training on hard surfaces e.g., concrete, also increases the risk of Achilles Tendinitis. Landing heavily or continuously on a hard surface can send a shock through the body which is partly absorbed by the Achilles tendon. A soft surface like grass turf helps to lessen the shock of the impact by absorbing some of the force of the feet landing heavily on the ground after a jump or during a running motion.
Symptoms
Symptoms of Achilles tendinitis and tendinosis include recurring localized heel pain, sometimes severe, along the achilles tendon during or after exercise. Pain often begins after exercise and gradually worsens. Morning tenderness or stiffness about an inch and a half above the point where the Achilles tendon is attached to the heel bone. Sluggishness in your leg. Mild to severe swelling. Stiffness that generally diminishes as the tendon warms up with use.
Diagnosis
On examination, an inflamed or partially torn Achilles tendon is tender when squeezed between the fingers. Complete tears are differentiated by sudden, severe pain and inability to walk on the extremity. A palpable defect along the course of the tendon. A positive Thompson test (while the patient lies prone on the examination table, the examiner squeezes the calf muscle; this maneuver by the examiner does not cause the normally expected plantar flexion of the foot).
Nonsurgical Treatment
Make sure that the tendon is not torn through and through. If it is severed, you must see a doctor immediately so that the tendon can be repaired. Severe injuries can sever a tendon, without a skin laceration being present. Testing involves moving the toes and foot to see if the tendon moves. If the tendon does not appear to move, it may be severed (comparing the injured tendon and its movement to the same tendon on the uninjured foot may help). Very sharp pain, a sudden pop, or an obvious gap in the structure of the tendon are all signs of a rupture, and should be seen by a doctor as soon as possible. If there is extreme swelling of the leg, and pain (out of proportion to the amount of trauma received), you may have sustained a vascular injury. A doctor must see this type of injury immediately. If you are not sure, see a doctor. If you have multiple injured areas see a doctor immediately, in order to prevent excessive swelling and pain. If the above exam is negative, then you may proceed with self-treatment. (However, if you are not sure of the extent of your injury, you should consult your doctor immediately). The sooner you begin to treat your injury by following "R.I.C.E.", the better you will feel. Rest is very important. Take off your shoe, get off your feet, and relax. Ice should be applied as soon as possible. Never apply ice directly on the injured area, as the cold may make the pain worse. Ice should be applied close to the injured site, between the heart and the injury, so that as the blood flows under the ice, it will be cooled. This cool blood flowing into the injured area will help to reduce the swelling and pain. Apply the ice, wrapped in a cloth or over an elastic bandage, to the foot for 15 minutes, every 1-2 hours, for up to 3 days after an injury. If the ice is uncomfortable, or causes increased pain, do not continue to use it, and see a doctor. If you have poor circulation do not use ice, as this may cause a serious problem. c. Compression is used to limit swelling, and to give support to the injured area. Compression should be applied to the entire foot, starting first at the toes and working back to the ankle. If it is applied just to the injured area, increased swelling will occur in front and behind the wrapping. Compression should be applied with a 3-inch elastic bandage, beginning around the base of all the toes, and then going around the foot and ankle. Continue over the calf muscle when possible. Compression reduces motion in the injured area and foot, and this decreases the pain, and allows for quicker healing. The bandage should not be so tight that it causes increased pain or throbbing in the toes or foot. It should be comfortable! Do not remove the elastic bandage for the first 12 hours, unless it becomes too tight, or the pain increases, or the toes become pale, blue, or cool. If any of these things happen, immediately remove all bandages, and leave them off for several hours. The normal color and temperature of the toes should return immediately. If not, see a doctor immediately! Continue until the swelling and pain subsides; it could take from several days to several weeks. d. Elevation of the leg will aid in reducing swelling and pain. Blood rushes to an injured area to bring increased blood cells, that aid in healing. Gravity will also force blood to the injured area. Too many cells and too much fluid will apply pressure to the injured nerves and tissues, and cause increased pain and delayed healing. Keep your foot elevated so that it is at least parallel to the ground, or higher if it is comfortable. Do this for at least 48 hours, or until the throbbing subsides, when you lower the leg.

Surgical Treatment
Mini-Open Achilles Tendon Repair. During a mini-open Achilles tendon repair surgery, 2 to 8 small stab incisions are made to pull the edges of the tendon tear together and suture the torn edges to repair the damage. During this procedure the surgeon will make one 3 to 4 cm long incision on the back of your ankle and 2 to 4 smaller vertical incisions around the long incision. These smaller veritical incisions are made with a pair of surgical scissors and are commonly referred to as "stab incisions". Once the incisions are opened up, the surgeon will place precise sutures with non-absorbable stitches to strengthen the damaged Achilles tendon tissue. This suturing technique reduces the amount of scar tissue on the tendon after surgery and provides better surface healing of the skin. Unlike the traditional method of an open surgery, this procedure has less risks and complications involved. To learn about all risks you may face be sure to speak to your doctor.
Prevention
Regardless of whether the Achilles injury is insertional or non-insertional, a great method for lessening stress on the Achilles tendon is flexor digitorum longus exercises. This muscle, which originates along the back of the leg and attaches to the tips of the toes, lies deep to the Achilles. It works synergistically with the soleus muscle to decelerate the forward motion of the leg before the heel leaves the ground during propulsion. This significantly lessens strain on the Achilles tendon as it decelerates elongation of the tendon. Many foot surgeons are aware of the connection between flexor digitorum longus and the Achilles tendon-surgical lengthening of the Achilles (which is done to treat certain congenital problems) almost always results in developing hammer toes as flexor digitorum longus attempts to do the job of the recently lengthened tendon. Finally, avoid having cortisone injected into either the bursa or tendon-doing so weakens the tendon as it shifts production of collagen from type one to type three. In a recent study published in the Journal of Bone Joint Surgery(9), cortisone was shown to lower the stress necessary to rupture the Achilles tendon, and was particularly dangerous when done on both sides, as it produced a systemic effect that further weakened the tendon.
What Leads To Heel Pain To Appear

Overview
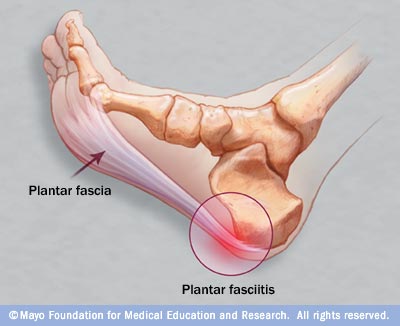
The plantar fascia is made up of 3 distinct parts: the medial, central, and lateral bands. The central plantar fascia is the thickest and strongest section, and this segment is also the most likely to be involved with plantar fasciitis. In normal circumstances, the plantar fascia acts like a windlass mechanism to provide tension and support through the arch. It functions as a tension bridge in the foot, providing both static support and dynamic shock absorption.
Causes
Plantar fasciitis is a painful disorder in the lower part of your foot usually around the heel. That pain usually hurts as you get up in the morning when you try to stand on your feet, or after any periods of inactivity. It is a disorder of a tough and strong band that connects the heel bone to the toes. Plantar Fasciitis is caused by injuring that tough band on the bottom of the foot. The following may be the causes of plantar fasciitis. Tight calf muscles or tight Achilles tendon produces repetitive over-stretching of the plantar fascia. Gait and balance Problem may be a dominant cause of this disorder. Many people have a special style of walking, with something unique that causes some kind of imbalance in their body. It might be something like locked knees, feet that turn-out, a weak abdomen etc. This imbalance may place some pressure on the fascia, which eventually causes plantar fasciitis. Weak foot muscles don’t give enough support to the plantar fascia. The small muscles in the foot give the foot its shape by keeping the bones in place and by expanding and contracting to make a movement. Weak foot muscles will allow greater stress on the fascia. Foot anatomical problems such as flat feet or high arches can make the fascia ligament work or stretch abnormally. Flattening of the fat pad at the sole of the feet under the heels is a Degeneration process that is caused by poor footwear or by age. Shoes that have no proper heel cup can flatten that fat pad quite quickly and cause this disorder. Walking in shoes which do not have good arch support is considered to be a cause of plantar fasciitis. Wearing inadequate or worn out shoes may place more stress on the fascia ligament. If you wear shoes that don't fit you by size or width, you may put your feet under excessive stress. Overweight Men and women are more vulnerable to developing the condition because of the excess weight on the foot. Pregnant women are at risk due to gaining weight through pregnancy and due to the pregnancy hormones that make ligaments loosen and relax. Sudden increase of activity like starting to run long distance or complete change of daily activity can cause heel pain and this disorder. Practice of repetitive athletic activities, like long distance running, playing a ball game, dancing or jumping, is a common cause for the disorder. Actually it is considered as one of the most common running injuries. Spending long periods of time on your feet everyday can cause plantar fasciitis. Working on your feet a few hours a day evey day may be the reason for your heel pain.
Symptoms
The typical presentation is sharp pain localized at the anterior aspect of the calcaneus. Plantar fasciitis has a partial association with a heel spur (exostosis); however, many asymptomatic individuals have bony heel spurs, whereas many patients with plantar fasciitis do not have a spur.
Diagnosis
The health care provider will perform a physical exam. This may show tenderness on the bottom of your foot, flat feet or high arches, mild foot swelling or redness, stiffness or tightness of the arch in the bottom of your foot. X-rays may be taken to rule out other problems.
Non Surgical Treatment
The key for the proper treatment of plantar fasciitis is determining what is causing the excessive stretching of the plantar fascia. When the cause is over-pronation (flat feet), an orthotic with rearfoot posting and longitudinal arch support is an effective device to reduce the over-pronation and allow the condition to heal. If you have usually high arches, which can also lead to plantar fasciitis, cushion the heel, absorb shock and wear proper footwear that will accommodate and comfort the foot. Other common treatments include stretching exercises, plantar fasciitis night splints, wearing shoes that have a cushioned heel to absorb shock, and elevating the heel with the use of a heel cradle or heel cup. Heel cradles and heel cups provide extra comfort, cushion the heel, and reduce the amount of shock and shear forces placed during everyday activities.

Surgical Treatment
If treatment hasn't worked and you still have painful symptoms after a year, your GP may refer you to either an orthopaedic surgeon, a surgeon who specialises in surgery that involves bones, muscles and joints, a podiatric surgeon, a podiatrist who specialises in foot surgery. Surgery is sometimes recommended for professional athletes and other sportspeople whose heel pain is adversely affecting their career. Plantar release surgery. Plantar release surgery is the most widely used type of surgery for heel pain. The surgeon will cut the fascia to release it from your heel bone and reduce the tension in your plantar fascia. This should reduce any inflammation and relieve your painful symptoms. Surgery can be performed either as, open surgery, where the section of the plantar fascia is released by making a cut into your heel, endoscopic or minimal incision surgery - where a smaller incision is made and special instruments are inserted through the incision to gain access to the plantar fascia. Endoscopic or minimal incision surgery has a quicker recovery time, so you will be able to walk normally much sooner (almost immediately), compared with two to three weeks for open surgery. A disadvantage of endoscopic surgery is that it requires both a specially trained surgical team and specialised equipment, so you may have to wait longer for treatment than if you were to choose open surgery. Endoscopic surgery also carries a higher risk of damaging nearby nerves, which could result in symptoms such as numbness, tingling or some loss of movement in your foot. As with all surgery, plantar release carries the risk of causing complications such as infection, nerve damage and a worsening of your symptoms after surgery (although this is rare). You should discuss the advantages and disadvantages of both techniques with your surgical team. Extracorporeal shockwave therapy (EST) is a fairly new type of non-invasive treatment. Non-invasive means it does not involve making cuts into your body. EST involves using a device to deliver high-energy soundwaves into your heel. The soundwaves can sometimes cause pain, so a local anaesthetic may be used to numb your heel. It is claimed that EST works in two ways. It is thought to, have a "numbing" effect on the nerves that transmit pain signals to your brain, help stimulate and speed up the healing process. However, these claims have not yet been definitively proven. The National Institute for Health and Care Excellence (NICE) has issued guidance about the use of EST for treating plantar fasciitis. NICE states there are no concerns over the safety of EST, but there are uncertainties about how effective the procedure is for treating heel pain. Some studies have reported that EST is more effective than surgery and other non-surgical treatments, while other studies found the procedure to be no better than a placebo (sham treatment).
What Can Cause Painful Heel To Flare Up

Overview
The plantar fascia is a strong, relatively inflexible, fibrous ligament band that runs through the bottom of the foot. That band helps to keep the complex arch system of the foot, absorb shock, plays a role in body balance and in the various phases of gait. The band transmits your weight across the bottom of the foot with each step you take. When the heel of the trailing leg starts to get off the ground, the band bears tension that is approximately twice the body weight. The tension on the band at this moment is even greater if the calf muscles are not flexible enough.
Causes
Under normal circumstances, your plantar fascia acts like a shock-absorbing bowstring, supporting the arch in your foot. If tension on that bowstring becomes too great, it can create small tears in the fascia. Repetitive stretching and tearing can cause the fascia to become irritated or inflamed.
Symptoms
If you have Plantar Fasciitis, you will most likely feel a sharp pain under the ball of you heel and it will often give pain when standing after a period of rest. For example when you get out of bed in the mornings or after being sat down. Some patients describe this feeling as a stone bruise sensation, or a pebble in the shoe and at times the pain can be excruciating. Patients with Plantar Fasciitis can experience pain free periods whereby the think they are on the mend, only for the heel pain to come back aggressively when they appear to have done nothing wrong. If your plantar fasciitis came on very suddenly and the pain is relentless, then you may have Plantar Fascial Tears. We will be able to differentiate between these 2 conditions, sometimes with ultra sound imaging. The treatment for each of these conditions will need to be very different.
Diagnosis
Plantar fasciitis is one of many conditions causing "heel pain". Some other possible causes include nerve compression either in the foot or in the back, stress fracture of the calcaneus, and loss of the fatty tissue pad under the heel. Plantar fasciitis can be distinguished from these and other conditions based on a history and examination done by a physician. It should be noted that heel spurs are often inappropriately thought to be the sole cause of heel pain. In fact, heel spurs are common and are nothing more than the bone's response to traction or pulling-type forces from the plantar fascia and other muscles in the foot where they attach to the heel bone. They are commonly present in patients without pain, and frequently absent from those who have pain. It is the rare patient who has a truly enlarged and problematic spur requiring surgery.
Non Surgical Treatment
Conservative treatment is almost always successful, given enough time. Traditional treatment often includes, rest, NSAIDs, and new shoes or heel inserts. Some doctors also recommend avoiding walking bare-footed. This means you’d have to wear your shoes as soon as you wake up. Certain foot and calf exercises are often prescribed to slowly build strength in the ligaments and muscles that support the arch of the foot. While traditional treatment usually relieves pain, it can last from several months to 2 years before symptoms get better. On average, non-Airrosti patients tend to get better in about 9 months.

Surgical Treatment
Most studies indicate that 95% of those afflicted with plantar fasciitis are able to relieve their heel pain with nonsurgical treatments. If you are one of the few people whose symptoms don't improve with other treatments, your doctor may recommend plantar fascia release surgery. Plantar fascia release involves cutting part of the plantar fascia ligament in order to release the tension and relieve the inflammation of the ligament. Overall, the success rate of surgical release is 70 to 90 percent in patients with plantar fasciitis. While the success rate is very high following surgery, one should be aware that there is often a prolonged postoperative period of discomfort similar to the discomfort experienced prior to surgery. This pain usually will abate within 2-3 months. One should always be sure to understand all the risks associated with any surgery they are considering.
Stretching Exercises
Exercises designed to stretch both your calf muscles and your plantar fascia (the band of tissue that runs under the sole of your foot) should help relieve pain and improve flexibility in the affected foot. A number of stretching exercises are described below. It's usually recommended that you do the exercises on both legs, even if only one of your heels is affected by pain. This will improve your balance and stability, and help relieve heel pain. Towel stretches. Keep a long towel beside your bed. Before you get out of bed in the morning, loop the towel around your foot and use it to pull your toes towards your body, while keeping your knee straight. Repeat three times on each foot. Wall stretches. Place both hands on a wall at shoulder height, with one of your feet in front of the other. The front foot should be about 30cm (12 inches) away from the wall. With your front knee bent and your back leg straight, lean towards the wall until you feel a tightening in the calf muscles of your back leg. Then relax. Repeat this exercise 10 times before switching legs and repeating the cycle. You should practise wall stretches twice a day. Stair stretches. Stand on a step of your stairs facing upstairs, using your banister for support. Your feet should be slightly apart, with your heels hanging off the back of the step. Lower your heels until you feel a tightening in your calves. Hold this position for about 40 seconds, before raising your heels back to the starting position. Repeat this procedure six times, at least twice a day. Chair stretches. Sit on a chair, with your knees bent at right angles. Turn your feet sideways so your heels are touching and your toes are pointing in opposite directions. Lift the toes of the affected foot upwards, while keeping the heel firmly on the floor. You should feel your calf muscles and Achilles tendon (the band of tissue that connects your heel bone to your calf muscle) tighten. Hold this position for several seconds and then relax. Repeat this procedure 10 times, five to six times a day. Dynamic stretches. While seated, roll the arch of your foot (the curved bottom part of the foot between your toes and heel) over a round object, such as a rolling pin, tennis ball or drinks can. Some people find that using a chilled can from their fridge has the added benefit of helping to relieve pain. Move your foot and ankle in all directions over the object for several minutes. Repeat the exercise twice a day.
What Causes Heel Discomfort To Flare Up
Overview
If your first few steps out of bed in the morning cause severe pain in the heel of your foot, you may have plantar fasciitis, an overuse injury that affects the sole of the foot. A diagnosis of plantar fasciitis means you have inflamed the tough, fibrous band of tissue (fascia) connecting your heel bone to the base of your toes.
Causes
Training on improper, hard and/or irregular surfaces as well as excessive track work in spiked shoes, or steep hill running, can stress the plantar fascia past its limits of elasticity, leading to injury. Finally, failure in the early season to warm up gradually gives the athlete insufficient time for the structures of the foot to re-acclimate and return to a proper fitness level for intensive exercise. Such unprepared and repeated trauma causes microscopic tearing, which may only be detected once full-blown plantar fasciitis and accompanying pain and debilitation have resulted. If the level of damage to the plantar fascia is significant, an inflammatory reaction of the heel bone can produce spike-like projections of new bone, known as heel spurs. Indeed, plantar fasciitis has occasionally been refereed to as heel spur syndrome, though such spurs are not the cause of the initial pain but are instead a further symptom of the problem. While such spurs are sometimes painless, in other cases they cause pain or disability in the athlete, and surgical intervention to remove them may be required. A dull, intermittent pain in the heel is typical, sometimes progressing to a sharp, sustained discomfort. Commonly, pain is worse in the morning or after sitting, later decreasing as the patient begins walking, though standing or walking for long periods usually brings renewal of the pain.
Symptoms
The heel pain characteristic of plantar fasciitis is usually felt on the bottom of the heel and is most intense with the first steps of the day. Individuals with plantar fasciitis often have difficulty with dorsiflexion of the foot, an action in which the foot is brought toward the shin. This difficulty is usually due to tightness of the calf muscle or Achilles tendon, the latter of which is connected to the back of the plantar fascia. Most cases of plantar fasciitis resolve on their own with time and respond well to conservative methods of treatment.
Diagnosis
Plantar fasciitis is one of many conditions causing "heel pain". Some other possible causes include nerve compression either in the foot or in the back, stress fracture of the calcaneus, and loss of the fatty tissue pad under the heel. Plantar fasciitis can be distinguished from these and other conditions based on a history and examination done by a physician. It should be noted that heel spurs are often inappropriately thought to be the sole cause of heel pain. In fact, heel spurs are common and are nothing more than the bone's response to traction or pulling-type forces from the plantar fascia and other muscles in the foot where they attach to the heel bone. They are commonly present in patients without pain, and frequently absent from those who have pain. It is the rare patient who has a truly enlarged and problematic spur requiring surgery.
Non Surgical Treatment
At the first sign of soreness, massage (roll a golf ball under your foot) and apply ice (roll a frozen bottle of water under your foot). What you wear on your feet when you're not running makes a difference. Arch support is key, and walking around barefoot or in flimsy shoes can delay recovery. If pain is present for more than three weeks, see a sports podiatrist. Treatments such as orthotics, foot taping, cortisone injections, night splints, and anti-inflammatories decrease symptoms significantly in about 95 percent of sufferers within six weeks. For more stubborn cases, physical therapy may be prescribed; six months of chronic pain may benefit from shock-wave therapy, an FDA-approved plantar-fasciitis treatment.

Surgical Treatment
Surgery is rarely needed in the treatment of plantar fasciitis. The vast majority of patients diagnosed with plantar fasciitis will recover given ample time. With some basic treatment steps, well over 90% of patients will achieve full recovery from symptoms of plantar fasciitis within one year of the onset of treatment. Simple treatments include anti-inflammatory medication, shoe inserts, and stretching exercises. In patients where a good effort with these treatments fails to provide adequate relief, some more aggressive treatments may be attempted. These include cortisone injections or extracorporeal shock wave treatments.
Stretching Exercises
In one exercise, you lean forward against a wall with one knee straight and heel on the ground. Your other knee is bent. Your heel cord and foot arch stretch as you lean. Hold for 10 seconds, relax and straighten up. Repeat 20 times for each sore heel. It is important to keep the knee fully extended on the side being stretched. In another exercise, you lean forward onto a countertop, spreading your feet apart with one foot in front of the other. Flex your knees and squat down, keeping your heels on the ground as long as possible. Your heel cords and foot arches will stretch as the heels come up in the stretch. Hold for 10 seconds, relax and straighten up. Repeat 20 times. About 90 percent of people with plantar fasciitis improve significantly after two months of initial treatment. You may be advised to use shoes with shock-absorbing soles or fitted with an off-the-shelf shoe insert device like a rubber heel pad. Your foot may be taped into a specific position. If your plantar fasciitis continues after a few months of conservative treatment, your doctor may inject your heel with steroidal anti-inflammatory medication. If you still have symptoms, you may need to wear a walking cast for two to three weeks or a positional splint when you sleep. In a few cases, surgery is needed for chronically contracted tissue.
What Can Cause Heel Discomfort

Overview
Plantar Fasciitis is the Latin term for "inflammation of the plantar fascia". The plantar fascia is a thick, fibrous ligament that runs under the foot from the heel bone to the toes. It forms the arch of the foot and functions as our natural shock-absorbing mechanism. Unlike muscle tissue, the plantar fascia is not very elastic and therefore is very limited in its capacity to stretch or elongate. Herein lies the problem, when too much traction is placed on the plantar fascia (for various reasons) micro-tearing will occur, resulting in irritation, inflammation and pain. Plantar Fasciitis usually causes pain under the heel. However some people may experience pain under the arch of the foot. Both heel pain and arch discomfort are related to Plantar Fasciitis, with heel pain being far more common than arch pain.
Causes
Plantar fasciitis most commonly occurs due to repetitive or prolonged activities placing strain on the plantar fascia. It is often seen in runners, or dancers and gymnasts who perform regular activities involving end of range foot and ankle movements. It may also occur in patients who walk excessively, especially up hills or on uneven surfaces. Older patients who spend a lot of time on their feet may also develop the condition. Plantar fasciitis frequently occurs in association with calf muscle tightness, inappropriate footwear, or biomechanical abnormalities, such as excessive pronation (flat feet) or supination (high arches). Occasionally the condition may occur suddenly due to a high force going through the plantar fascia beyond what it can withstand. This may be due to activities such as a sudden acceleration or a forceful jump.
Symptoms
Most people with plantar fasciitis have pain when they take their first steps after they get out of bed or sit for a long time. You may have less stiffness and pain after you take a few steps. But your foot may hurt more as the day goes on. It may hurt the most when you climb stairs or after you stand for a long time. If you have foot pain at night, you may have a different problem, such as arthritis, or a nerve problem such as tarsal tunnel syndrome.
Diagnosis
During the physical exam, your doctor checks for points of tenderness in your foot. The location of your pain can help determine its cause. Usually no tests are necessary. The diagnosis is made based on the history and physical examination. Occasionally your doctor may suggest an X-ray or magnetic resonance imaging (MRI) to make sure your pain isn't being caused by another problem, such as a stress fracture or a pinched nerve. Sometimes an X-ray shows a spur of bone projecting forward from the heel bone. In the past, these bone spurs were often blamed for heel pain and removed surgically. But many people who have bone spurs on their heels have no heel pain.
Non Surgical Treatment
Cut back on walking, running or athletic weight bearing activities. Try the recommended stretches above. Shoes with a good arch support and heel cushioning or over-the-counter orthotics may help. Icing the area of pain or taking a short course of anti-inflammatory medications such as ibuprofen or acetaminophen will help with pain. If treatments do not help, a doctor can suggest other options.

Surgical Treatment
In very rare cases plantar fascia surgery is suggested, as a last resort. In this case the surgeon makes an incision into the ligament, partially cutting the plantar fascia to release it. If a heel spur is present, the surgeon will remove it. Plantar Fasciitis surgery should always be considered the last resort when all the conventional treatment methods have failed to succeed. Endoscopic plantar fasciotomy (EPF) is a form of surgery whereby two incisions are made around the heel and the ligament is being detached from the heel bone allowing the new ligament to develop in the same place. In some cases the surgeon may decide to remove the heel spur itself, if present. Just like any type of surgery, Plantar Fascia surgery comes with certain risks and side effects. For example, the arch of the foot may drop and become weak. Wearing an arch support after surgery is therefore recommended. Heel spur surgeries may also do some damage to veins and arteries of your foot that allow blood supply in the area. This will increase the time of recovery.
Stretching Exercises
Exercises designed to stretch both your calf muscles and your plantar fascia (the band of tissue that runs under the sole of your foot) should help relieve pain and improve flexibility in the affected foot. A number of stretching exercises are described below. It's usually recommended that you do the exercises on both legs, even if only one of your heels is affected by pain. This will improve your balance and stability, and help relieve heel pain. Towel stretches. Keep a long towel beside your bed. Before you get out of bed in the morning, loop the towel around your foot and use it to pull your toes towards your body, while keeping your knee straight. Repeat three times on each foot. Wall stretches. Place both hands on a wall at shoulder height, with one of your feet in front of the other. The front foot should be about 30cm (12 inches) away from the wall. With your front knee bent and your back leg straight, lean towards the wall until you feel a tightening in the calf muscles of your back leg. Then relax. Repeat this exercise 10 times before switching legs and repeating the cycle. You should practise wall stretches twice a day. Stair stretches. Stand on a step of your stairs facing upstairs, using your banister for support. Your feet should be slightly apart, with your heels hanging off the back of the step. Lower your heels until you feel a tightening in your calves. Hold this position for about 40 seconds, before raising your heels back to the starting position. Repeat this procedure six times, at least twice a day. Chair stretches. Sit on a chair, with your knees bent at right angles. Turn your feet sideways so your heels are touching and your toes are pointing in opposite directions. Lift the toes of the affected foot upwards, while keeping the heel firmly on the floor. You should feel your calf muscles and Achilles tendon (the band of tissue that connects your heel bone to your calf muscle) tighten. Hold this position for several seconds and then relax. Repeat this procedure 10 times, five to six times a day. Dynamic stretches. While seated, roll the arch of your foot (the curved bottom part of the foot between your toes and heel) over a round object, such as a rolling pin, tennis ball or drinks can. Some people find that using a chilled can from their fridge has the added benefit of helping to relieve pain. Move your foot and ankle in all directions over the object for several minutes. Repeat the exercise twice a day.
Symptoms Of Drop Foot
Did you know that redheads require 20% more general anesthesia than non-gingers before going under the knife? Often taken for granted, our feet and ankles are subjected to a rigorous workout everyday. Pain, such as may occur in our heels, alerts Foot Callous us to seek medical attention. The fungal problems seen most often are athlete's foot and fungus nails. Big toe joint pain can be a warning sign of arthritis. Enter the shape, color, or imprint of your prescription or OTC drug. Help!!!!!
If changing your shoes isn't helping to solve your foot pain, it is time for us to step in. Contact Dr. Jeff Bowman at Houston Foot Specialists for treatment that will keep your feet feeling great. Inserting arch support insoles in the shoes is also a good option.
Pain often occurs suddenly and mainly around the undersurface of the heel, although it often spreads to your arch. The condition can be temporary, but may become chronic if you ignore it. Resting usually provides relief, but the pain may return. Heel spurs are bony growths that protrude from the bottom of the heel bone, and they are parallel to the ground. There is a nerve that runs very close to this area and may contribute to the pain which occurs.
On the other hand, the surgical hip pain treatment includes total hip bone replacement surgery. Although it is always advisable to consult the doctor if you experience pain in the hip that lasts for more than a couple of hours, you can try some home remedies to temporarily get rid of the sharp hip pain. One should note that these home remedies are not to be substituted for proper medical treatment. Ice packs and cool compresses are helpful to ease pain and inflammation on various parts of the body. Rest and ice the sole of your feet.
During the average lifetime our feet cover over 70,000 miles, the equivalent of walking four times around the world., so it's not surprising that problems can occur. Indeed around three-quarters of all adults will experience some sort of problem with their feet at some time. And without treatment most foot complaints will become gradually worse with time. This means people often endure painful conditions for far too long, and the problem can get worse. People often assume nothing can be done to help their condition, but in fact these conditions are extremely treatable. Swollen lump on big toe joint; lump may become numb but also make walking painful.
If changing your shoes isn't helping to solve your foot pain, it is time for us to step in. Contact Dr. Jeff Bowman at Houston Foot Specialists for treatment that will keep your feet feeling great. Inserting arch support insoles in the shoes is also a good option.
Pain often occurs suddenly and mainly around the undersurface of the heel, although it often spreads to your arch. The condition can be temporary, but may become chronic if you ignore it. Resting usually provides relief, but the pain may return. Heel spurs are bony growths that protrude from the bottom of the heel bone, and they are parallel to the ground. There is a nerve that runs very close to this area and may contribute to the pain which occurs.

On the other hand, the surgical hip pain treatment includes total hip bone replacement surgery. Although it is always advisable to consult the doctor if you experience pain in the hip that lasts for more than a couple of hours, you can try some home remedies to temporarily get rid of the sharp hip pain. One should note that these home remedies are not to be substituted for proper medical treatment. Ice packs and cool compresses are helpful to ease pain and inflammation on various parts of the body. Rest and ice the sole of your feet.

During the average lifetime our feet cover over 70,000 miles, the equivalent of walking four times around the world., so it's not surprising that problems can occur. Indeed around three-quarters of all adults will experience some sort of problem with their feet at some time. And without treatment most foot complaints will become gradually worse with time. This means people often endure painful conditions for far too long, and the problem can get worse. People often assume nothing can be done to help their condition, but in fact these conditions are extremely treatable. Swollen lump on big toe joint; lump may become numb but also make walking painful.
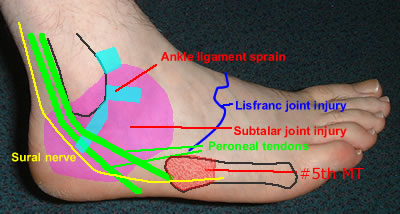
Print "Symptoms Associated With Side Of Foot Pain"
You may have plantar fasciitis, a painful condition that is very common in runners or people who stand on their feet for long periods. Foot pain can inhibit a person from doing even the simplest activities, such as playing on the beach, washing dishes, or taking a walk with family members. Kids can experience foot pain for a lot of reasons. Sometimes you may feel as if your feet is on fire.
Well, Mimi, we still have the same effective Walkfit design as before but we've added two significant changes. We added a specialized gel pad where it counts most, directly under the heel. I'd get a pair of Walkfits just to keep my feet fresh and I'd give a pair to everyone I know. It supports both sides and the back of your foot to help lock the foot in and keep the heel from rolling. And most important, the Walkfit flexes to help absorb shock and then returns the energy to your foot to help you walk. Your foot actually conforms to the Walkfit, not the other way around. It's like those back chairs that place your back and spine in the correct position to alleviate the pressure and the pain, and the Walkfit does the same for your feet. Along with the new gel pad, we now have an orthotic that protects, stabilizes, cushions and absorbs shock like nothing else. If I don't wear 'em, then my feet ache again.
Athletes foot is a common skin condition causing itchy, flaky skin and a burning sensation usually between the toes. Flat feet are usually the result of one's own genetics inherited from their family. Flattening is a normal part of the walking cycle of the foot, and in fact this is how the body disperses much of the shock forces created with walking. However, in some individuals, the foot flattens outward too much. This changes the way certain muscles in the foot and leg have to function, which causes numerous changes to the feet over time. These changes can include chronic straining of ligaments and tendons, as well as the development of deformities that rely on structural imbalance like bunions and hammertoes. There are numerous ways to treat flat feet.
Whether you have bunions, high arches, or anything in between, be sure to visit USA Orthotics USA Orthotics is one of the top manufacturers or custom orthotics, and they can make a mold specifically for your foot. Wear comfortable shoes that provide the right kind of support for your feet.
One of the most common causes is improper walking habits, i.e., exerting weight or pressure on the metatarsals while walking or running which can lead to pain at night. Symptoms include sharp pain in the middle part of the foot, callousing around the toes, and tingling sensation and severe pain while walking or standing. Pain in the middle of the leg, i.e. in the metatarsals is also one of the symptoms of arthritis.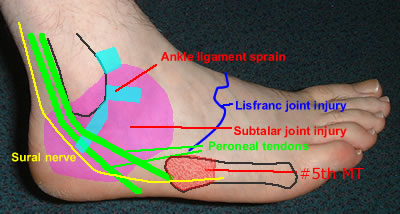
I think your website is the most informative site I have found when researching foot pain. I used to work for a podiatrist (front desk) back during summers in college years ago, so I know the benefits of good care. It was so great to get to your site (top of google search) and actually find all the answers I needed EASILY and QUICKLY! I have been experiencing foot pain of various sorts and am working to figure out what it is. I found this site and can only say BRAVO!! The pain finally brought me to the ER. I spent 8 days in the hospital. It can also assist in reducing pain levels.
Light and washable, they also have specially designed air vents to help keep your feet cool. We'll also include this bottle of soothing peppermint lotion to invigorate your feet and your spirit... And our special sandal adapters, so you'll never be without your Walkfits. It inhibits and kills fungus and bacteria, so no more stinky, sticky feet. And don't forget, we have holes in the Walkfit to keep your feet cool all the time.
Well, Mimi, we still have the same effective Walkfit design as before but we've added two significant changes. We added a specialized gel pad where it counts most, directly under the heel. I'd get a pair of Walkfits just to keep my feet fresh and I'd give a pair to everyone I know. It supports both sides and the back of your foot to help lock the foot in and keep the heel from rolling. And most important, the Walkfit flexes to help absorb shock and then returns the energy to your foot to help you walk. Your foot actually conforms to the Walkfit, not the other way around. It's like those back chairs that place your back and spine in the correct position to alleviate the pressure and the pain, and the Walkfit does the same for your feet. Along with the new gel pad, we now have an orthotic that protects, stabilizes, cushions and absorbs shock like nothing else. If I don't wear 'em, then my feet ache again.
Athletes foot is a common skin condition causing itchy, flaky skin and a burning sensation usually between the toes. Flat feet are usually the result of one's own genetics inherited from their family. Flattening is a normal part of the walking cycle of the foot, and in fact this is how the body disperses much of the shock forces created with walking. However, in some individuals, the foot flattens outward too much. This changes the way certain muscles in the foot and leg have to function, which causes numerous changes to the feet over time. These changes can include chronic straining of ligaments and tendons, as well as the development of deformities that rely on structural imbalance like bunions and hammertoes. There are numerous ways to treat flat feet.
Whether you have bunions, high arches, or anything in between, be sure to visit USA Orthotics USA Orthotics is one of the top manufacturers or custom orthotics, and they can make a mold specifically for your foot. Wear comfortable shoes that provide the right kind of support for your feet.
One of the most common causes is improper walking habits, i.e., exerting weight or pressure on the metatarsals while walking or running which can lead to pain at night. Symptoms include sharp pain in the middle part of the foot, callousing around the toes, and tingling sensation and severe pain while walking or standing. Pain in the middle of the leg, i.e. in the metatarsals is also one of the symptoms of arthritis.
I think your website is the most informative site I have found when researching foot pain. I used to work for a podiatrist (front desk) back during summers in college years ago, so I know the benefits of good care. It was so great to get to your site (top of google search) and actually find all the answers I needed EASILY and QUICKLY! I have been experiencing foot pain of various sorts and am working to figure out what it is. I found this site and can only say BRAVO!! The pain finally brought me to the ER. I spent 8 days in the hospital. It can also assist in reducing pain levels.
Light and washable, they also have specially designed air vents to help keep your feet cool. We'll also include this bottle of soothing peppermint lotion to invigorate your feet and your spirit... And our special sandal adapters, so you'll never be without your Walkfits. It inhibits and kills fungus and bacteria, so no more stinky, sticky feet. And don't forget, we have holes in the Walkfit to keep your feet cool all the time.